It is not uncommon for individuals with torn rotator cuff tendons to endure the pain, develop arthritis and end up with a condition they can’t ignore: pseudo-paralysis — where they can’t move their arm. According to Paul Re, MD, orthopedic surgeon, reverse shoulder surgery was developed for these patients. As the surgery evolved, outcomes have improved. Dr. Re is one of very few surgeons outside of Boston using a CT-guided implant positioning system to plan patient-specific surgery.
Long before anyone attempted hip or knee replacement surgery, the focus was on shoulder replacement — a way to keep the body’s most complicated joint working. Progress in surgical technique and implant design led to predictable success, but by the 1980s, it was clear that outcomes are less likely when the rotator cuff is not functional.
“For patients with rotator cuff arthropathy, we try anti-inflammatories, physical therapy and injections,” says Dr. Re, “but when nothing controls their pain, they’re unable to sleep or they have a pseudoparalyzed, non-functional arm, reverse shoulder surgery can be the right option.”
The procedure reverses the location of the shoulder components, with the metal ball screwed into the glenoid, and the plastic cup secured into the humerus. In the absence of a healthy rotator cuff, reverse shoulder surgery relies on the deltoid muscle. “If a patient has a torn rotator cuff, and I perform traditional shoulder replacement surgery, the shoulder is still dislocated superiorally,” Dr. Re explains. “That’s where the reverse shoulder comes in. It allows the deltoid to provide the necessary motion.
“During the past 20 years, the components have become far more anatomic,” he adds. “As a result, the complication rate has been reduced from 10 percent to 2 percent, and many more patients are choosing it. Today, about half of the shoulder replacements I perform are reverse shoulders.”
A 3D model for patient-specific surgery
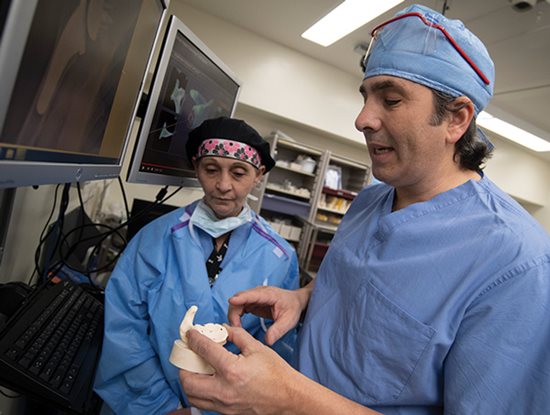
Another advance has helped drive down the complication rate: the use of CT scans to construct a 3D model of the patient’s anatomy. “Prior to surgery, we use it to build a guide system for placement of wires,” says Dr. Re (
shown at right looking at a 3D model with Karen Robinson, RN, RNFA). “Once the procedure has begun, we cut the humeral head to obtain the bone graft and then use the 3D model to precisely position the shoulder components.”
In addition to the reduction in complications, Dr. Re says this new approach to performing reverse shoulder surgery produces better motion than was possible before. “I performed my first reverse shoulder surgery 18 years ago,” he notes. “At the time, reverse shoulders often were salvage procedures. There was nothing else to offer patients.”
Today, his patients who receive successful reverse shoulder replacements are predictably pleased. “They’re my happiest patients, because they are out of pain and regain function. Unlike other shoulder surgeries, where we operate on torn tendons that are raw and irritated, shoulder replacement surgery replaces painful surfaces with smooth surfaces. Patients experience a great deal of relief.”
In general, individuals with chronic shoulder pain are interested in maintaining their independence. “These patients tend to be in their 70s or older,” says Dr. Re. “They tell me they want to stay in their homes, so they need to be able to drive and cook. This isn’t about playing tennis. They may be able to golf, but we don’t encourage tennis after shoulder replacement surgery.”
Dr. Re emphasizes that torn rotator cuffs should not be ignored. “They can turn into worse problems,” he notes. “It is easier to repair a tear when it is small. We can stop the pain and the tear from progressing to where it is too large to fix.”
Also, he is quick to point out that reverse shoulder surgery is never option one for patients with rotator cuff arthropathy. “It may be option five, after trying various conservative treatments. I have patients who I see every three or four months. They are doing well with pain injections and exercises. That is all they need.”
A recent patient exemplifies the effectiveness of successful reverse shoulder surgery. “She is an 84-year-old woman who developed arthritis and pseudo-paralysis. For whatever reason, she did not have her rotator cuff repaired when she developed a tear, and it had grown in size. This patient, who told me she wanted to remain as independent as possible, was back to driving and teaching four weeks after we performed her reverse shoulder surgery.”

